
You are reading:

You are reading:
21.02.25
9 minutes readThe diagnosis of a rare disease can take an average of five years – a wait that, in many cases, does not lead to an immediate solution, as 95% of these conditions still have no cure. In search of answers for the more than three million people affected in Spain, we spoke with the chief executive officer of Hospital Sant Joan de Déu, one of Europe’s leading centres for the diagnosis and treatment of rare diseases, as well as with two researchers supported by the CaixaResearch Health and CaixaImpulse Health Innovation calls, who are working to shed light on a field where much remains unknown.
Rare diseases are uncommon conditions that affect fewer than five people per 10,000 inhabitants. Currently, more than 7,000 rare diseases have been identified – new ones are described every year – and it is estimated that around 300 million people worldwide live with a rare disease. The vast majority, up to 95%, still have no specific pharmaceutical treatment or cure.
According to the Spanish Federation of Rare Diseases (FEDER), patients can wait up to five years to receive an accurate diagnosis of what is happening to them. In 20% of cases it can take more than 10 years. When that moment arrives, the impact is profound, both for the person affected and their family.
Dr Manel del Castillo, CEO of Hospital Sant Joan de Déu in Barcelona, explains: “Few hospitals are equipped to care for patients with a rare disease. When a diagnosis is finally made, most families have to move and live in another city for treatment, moving away from their family support network, which makes coping with the situation even more difficult.”

Eighty per cent of patients develop symptoms in childhood. Moreover, most rare diseases are chronic and degenerative, leading to a high level of dependency. “We’re talking about very severe conditions; in fact, at present, one in three children affected by these diseases does not reach the age of five,” says Del Castillo, whose hospital is Spain’s leading reference centre for treating these conditions in children.
In the field of rare diseases, research projects go beyond achieving scientific results. Advances have a significant impact on patients’ quality of life and life expectancy, while also providing crucial information and support to families once they receive a diagnosis. In this report, we explore two projects that aim to shed light on two of these diseases.
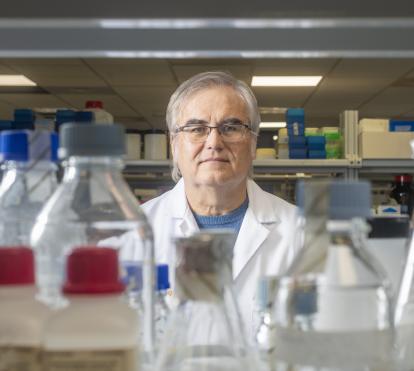
Ataxias are a very broad and heterogeneous group of rare neurodegenerative diseases that primarily affect the cerebellum, the spinal cord and the nerves responsible for muscle contractions, and thus the movement of limbs. One of the most common types is Friedreich’s ataxia, caused by a genetic alteration that leads to severe progressive neurodegeneration, cardiac involvement and movement disorders.

As explained by Antoni Matilla, researcher at the Germans Trias i Pujol Research Institute (IGTP) and co-founder of the company Biointaxis S.L., whose project has received two grants from CaixaImpulse Health Innovation, “The disease onset varies, appearing in childhood or adolescence, depending on the patient. The affected person begins to notice a loss of sensation in their legs, experiences difficulty walking, stumbles, falls, and then seeks medical attention from a neurologist. Faced with this motor incoordination, the neurologist may request genetic testing to confirm a suspected diagnosis of ataxia,” he explains.
Friedreich’s ataxia is caused by a mutation in the FXN gene, located on chromosome 9. This mutation leads to a deficiency in the production of a protein called frataxin, which is essential for normal cell function. This deficiency, in turn, causes a high and toxic accumulation of iron within the cells, leading to cellular damage and mitochondrial dysfunction
For over 10 years, Dr Matilla’s team has been working on designing viral DNA sequences to replace the damaged ones. “We’ve developed a strategy to replace frataxin protein levels using a recombinant adeno-associated virus, from which we have removed all potentially toxic or abnormal sequences in order to effectively distribute the protein we’re interested in,” he explains.
The validation of this drug’s safety is in the hands of Biointaxis, a spin-off of IGTP established in 2018, which has led the preclinical phase – conducted before human trials – which was completed last year. Experts are highly satisfied with the results and anticipate that clinical trials in humans could begin in 2026. “The BTX-101 compound, based on adeno-associated viruses (AAV), has shown excellent results in two mouse models, with recovery in nearly 90% of cases, both in the acute and chronic phases of the disease,” says Matilla. More recently, Biointaxis scientists have demonstrated its feasibility and safety in non-human primates

“Therefore,” adds the expert, “based on the results we have so far, we’re talking about a fully curative therapy. On the one hand, we could prevent patients from developing the disease, and on the other, significantly improve symptom management for those who already have it and, consequently, their quality of life.”
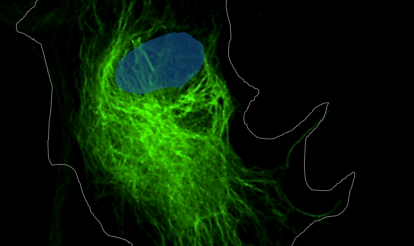
Alexander disease is a rare disorder classified as a leukodystrophy, a group of conditions characterised by the destruction of the myelin sheaths that protect nerve fibres and enable the rapid and normal transmission of nerve impulses. This disorder is caused by mutations in the glial fibrillary acidic protein (GFAP), which is found in astrocytes, a type of cell essential for the proper functioning of the central nervous system.

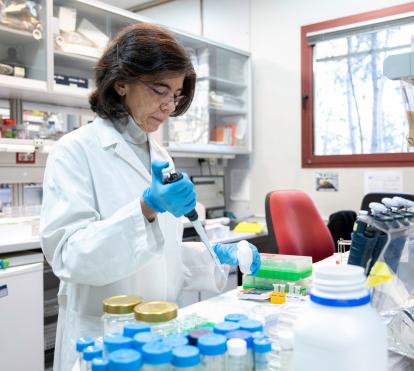
Symptoms vary depending on the type of mutation and the patient’s age. However, certain signs and symptoms can help identify the condition, such as developmental delays in infants and children, seizures, spasticity, ataxia (loss of coordination and balance), speech and language difficulties, and even macrocephaly or hydrocephalus. As researcher Dolores Pérez-Sala explains, “The age of onset of symptoms in Alexander disease is highly variable, ranging from just a few months of life to much later ages. In general, the earlier the disease manifests, the worse the prognosis.”
Diagnostic techniques have improved in recent years, making it possible to detect more cases of this disease. “In adults, mild or non-specific symptoms may appear, often mistaken for those of other neurodegenerative diseases. Thanks to recent advances, some disorders that previously had an unknown cause can now be diagnosed as Alexander disease,” she emphasises.
The team at the Margarita Salas Center for Biological Research, of the Spanish National Research Council (CSIC), led by Pérez-Sala and supported by funding from CaixaResearch Health, is developing a project in collaboration with national and international research groups to investigate how GFAP mutations lead to significant damage in both astrocytes and neurons.
As the researcher points out, “We’ve obtained results indicating that many astrocyte functions are disrupted, and there’s reduced resistance to stress. This has validated our initial hypothesis: the GFAP mutation leads to cellular damage, but in turn, the cellular damage further deteriorates the mutant protein.” They have now begun testing potential protective strategies for the alterations they have identified, first using cell models and then moving on to more complex models.
The initial results provide a molecular explanation for some aspects of the disease’s progression. As Pérez-Sala explains, “The disease worsens when the patient experiences intense stress affecting the brain, such as a very high fever or a traumatic brain injury, etc.”
This study will also help improve understanding of the mechanisms involved in other common neurodegenerative diseases. “Alexander disease shares several characteristics with conditions such as Alzheimer’s disease, amyotrophic lateral sclerosis (ALS) and even issues resulting from trauma or strokes. That’s why we hope our findings may also be useful in the fight against these diseases,” the expert predicts.

Although the current treatment for this disease is primarily symptomatic and tailored to each patient, a clinical trial is currently underway with an experimental drug designed to inhibit GFAP production. In preclinical phases, it has shown very promising results. “The goal is to reduce the levels of the abnormal protein to prevent it from significantly impairing cell function. The results, at least regarding the drug’s safety, are expected by the end of this year,” reveals Pérez-Sala
Experts agree that researching rare diseases presents a significant challenge. According to Matilla, “The main obstacle we face in advancing the diagnosis and treatment of rare diseases is funding. Fortunately, I believe that more and more pharmaceutical companies are investing in the development of drugs and therapies for rare diseases. But research funding is still not at the level of other, much more common conditions, such as HIV or cancer.”
As Del Castillo explains, “Research is essential for achieving faster diagnoses and improving treatments. To do this, we need talent, facilities and financial resources, which is why collaboration with the ”la Caixa” Foundation is crucial to continue making progress in this field.”
Over the past 10 years, the ”la Caixa” Foundation has supported more than 45 research and innovation projects on rare diseases. Additionally, it has recently allocated 7.5 million euros to boost research into paediatric rare diseases at Hospital Sant Joan de Déu. This partnership has a twofold objective: to improve diagnosis through machine learning and artificial intelligence techniques to group and analyse large datasets, and thus to facilitate the research of new treatments.
In addition to the need for improved resources, Pérez-Sala acknowledges that the low prevalence of these diseases in the population can make it difficult to obtain a sufficient amount of data. “It’s also challenging to develop suitable experimental models, especially in cases where the cause of the disease is unknown or when dealing with multifactorial diseases. This presents an additional challenge in the search for potential treatments.”
For Del Castillo, if we want the future of these diseases to be better than the present, “We have to achieve integrated centres that provide more comprehensive care for patients; more translational centres that can combine clinical care and research; and more cooperative centres that involve society as a whole, other research institutions and families in the search for solutions.”