
You are reading:

You are reading:

28.02.24
6 minutes readEvery year, 28,000 premature babies are born in Spain, 800 of them extremely premature with a higher risk of suffering complications or not surviving. BCNatal, which integrates functionally the Maternal-Fetal Medicine and Obstetrics Departments of Sant Joan de Déu Hospital and the Hospital Clínic, is working with the support of the ”la Caixa” Foundation on the prototype of an artificial placenta that attempts to reproduce the physiological conditions of the womb to help the organs of extremely premature babies mature, reduce complications and improve their life expectancy.
Is it possible to develop an artificial placenta for extremely premature newborns that allows the foetus to be kept outside the mother’s womb in an environment that’s as similar as possible to it, thus minimising the risk of complications? This question could represent a huge leap forward for science in terms of the survival of extremely premature babies and is the starting point for CaixaResearch Artificial Placenta, an initiative led by Dr Eduard Gratacós, director of BCNatal.
This is the first experimental project of an artificial placenta in an animal model in Europe, and focuses on extremely premature babies born between 23 and 28 weeks of gestation instead of the desired 40 weeks. These babies weigh between 500 and 700 grams and have a life expectancy rate of between 25% and 75%, depending on their prematurity. If they survive, they usually suffer serious consequences for the rest of their lives, such as pulmonary, infectious, cognitive, motor and other issues.
There are many reasons for preterm birth. Most are spontaneous, but many are due to medical reasons such as infections or other pregnancy complications that require early induction of labour. They are also linked to multiple pregnancies or chronic conditions like diabetes and high blood pressure. Genetic causes may also be involved.
Fortunately, we’re on the way to a solution. “There has been no increase in survival rates for these babies for 20 years, because despite having highly developed technology, there’s a biological limit determined by the premature baby’s own organs, which are not yet ready to function,” says Elisenda Eixarch, senior specialist at BCNatal and scientific coordinator of the project. For this reason, the research team – made up of more than 35 professional from various disciplines – is striving to make both the artificial uterus and the placental functions of the artificial placenta as similar as possible to biological organs.


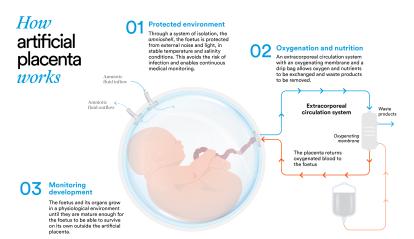
The role of the placenta is key to foetal development. “It’s where maternal and foetal blood meet, although they never actually touch. It works like the circuits of a radiator: in this parallel circulation, with circuits so close to each other, oxygen, nutrients and all the substances produced by the placenta are transferred to the foetus. One of the most surprising facts about the placenta is that it’s the only temporary organ in the human body. When a baby is born prematurely, the placenta disappears prematurely along with its functions of protection and vital development of the foetus,” explains Eixarch. “In order to replicate this organ, we’ve created an extracorporeal circulation system with tubes that we connect to the foetus’ umbilical cord to supply it with oxygen and nutrients.”

A kind of sack has also been created to enclose and protect the foetus: the amnioshell. “It’s a transparent container that closes with a lid and allows us to keep the foetus in an environment that’s isolated from noise and light, with stable temperature conditions and preventing it from becoming infected. We can see how the foetus is from the outside and do ultrasound scans, but it’s isolated,” she says. It also has permanent monitoring systems and, as Eixarch points out, “is a completely different concept from that of an incubator. Incubators are simply a place where the baby is warm and humid, [but] where it has to breathe and feed on its own, unlike the amnioshell.”
The most delicate operation for the team is the transition from the womb to the artificial placenta. The aim is that the baby does not notice it’s changing from a foetus to a life in the artificial placenta, that it feels like it’s still in the womb, in its natural environment. The researcher explains the details: “The key moment is when we cannulate the vessels in the umbilical cord: we insert the cannulas of our system inside them. We have to do this very quickly and carefully to avoid any complications. Despite it being such a critical moment, we’ve managed to do it very well. In the past year, the transitions performed have been successful,” she adds.


Finally, when the foetus is ready, the most birth-like moment comes: transfer of the baby from the amnioshell to neonatal life. “When we cut the umbilical cord, the foetus notices it and we have to act quickly,” says Eixarch.
Despite these successes, the project is still at an early stage. They have created a first prototype and there’s still a lot of work to be done. “The goal is to create a solid solution and to do this we need to make some modifications to the system: improve the oxygenating membrane and further refine the cannulation technique,” says the project’s scientific coordinator. “We’re now working to increase the survival time in good foetal condition in the animal model from the current 12 days to three or four weeks. Once we’ve achieved this and our prototype is more robust and stable, we’ll be ready for the first clinical study in humans, which we expect to take place in two or three years”. To this end, the ”la Caixa” Foundation is supporting the project with 4.3 million euros, in addition to the 3.35 million granted for the first phase, now completed and evaluated. This additional funding will allow the project to move on to phase two.
From here, the applications could be endless. For example, this artificial placenta could enable foetal heart operations that cannot be performed today. “It’s still very difficult to imagine all the applications, but we know that there are conditions that will certainly benefit from this solution,” concludes Eixarch, who describes the project as “an absolute challenge”. “I still remember the day when Dr Gratacós proposed that I become the coordinator, and I thought: ‘How can I say no? This is the project of my life, an incredible opportunity to be part of something that’s going to change the way we do medicine and change people’s lives. Especially the lives of the 25,000 extremely premature babies born in Europe every year and their families.’”